Queensland : A Grim Health Warning from Queensland Futures Forum
Queensland
Queensland’s top health think tank has issued a sobering alert: children in some regions may not live as long as their parents. At a recent Queensland Futures Institute forum, Dr Robyn Littlewood, CEO of Health and Wellbeing Queensland, revealed a plunging median death age—dropping as low as fifty‑two in Far North Queensland—compared to eighty‑two in Brisbane. This signals was a crisis in child health, driven by rising chronic illnesses.
Even more worryingly, Dr Littlewood emphasised that a large portion of these conditions is preventable. She reported that ninety percent of childhood type two, eighty percent of heart illness, and forty percent of cancers could be avoided through early intervention. Consequently, experts are calling for urgent system overhaul.
Chronic Disease Crisis Among Young Queenslanders
Once rare, chronic conditions are now alarmingly common among children. Type two, fatty liver, high cholesterol, and paediatric obesity are surging across the state . Shockingly, prescriptions for Ozempic to manage childhood diabetes have increased tenfold in four years, highlighting how dramatically trends are shifting.
Given that half of all Queenslanders now live with at least one chronic disease, childhood interventions cannot wait. Families and policymakers alike are waking to the idea that today’s youth may inherit lifelong health battles.
Queensland Alarm : The Preventable Toll on Future Generations
Dr Littlewood warned that if no action is taken, chronic conditions could begin in childhood and escalate, causing young Queenslanders to endure multiple illness. During the forum, she asked the audience: isn’t it outrageous to think a child may die younger than the previous generation? .
Amid this crisis, cost‑effective prevention showed promise. “Wellness My Way” digital health pilots, implemented in Roma, Bundaberg, and Logan, have attracted hundreds of families. These initiatives offer health coaching and lifestyle guidance, driving down hospital admissions and improving engagement.
Workforce Strain Hampers Prevention Efforts
Yet the system struggles to keep up. According to Noelle Cridland, Metro South Health’s chief executive, seventy‑five percent of nurses and midwives are working part‑time, complicating efforts to deliver consistent care. To address shortages, medical documentation is being streamlined with AI, and non‑doctor clinicians are gaining new responsibilities, including prescribing authority.
Universities are also stepping in. In rural areas like Charleville, remote nursing students enter the workforce and stay, offering hope that education tied to local training can help fill care gaps .
Regional Highlight Urgency
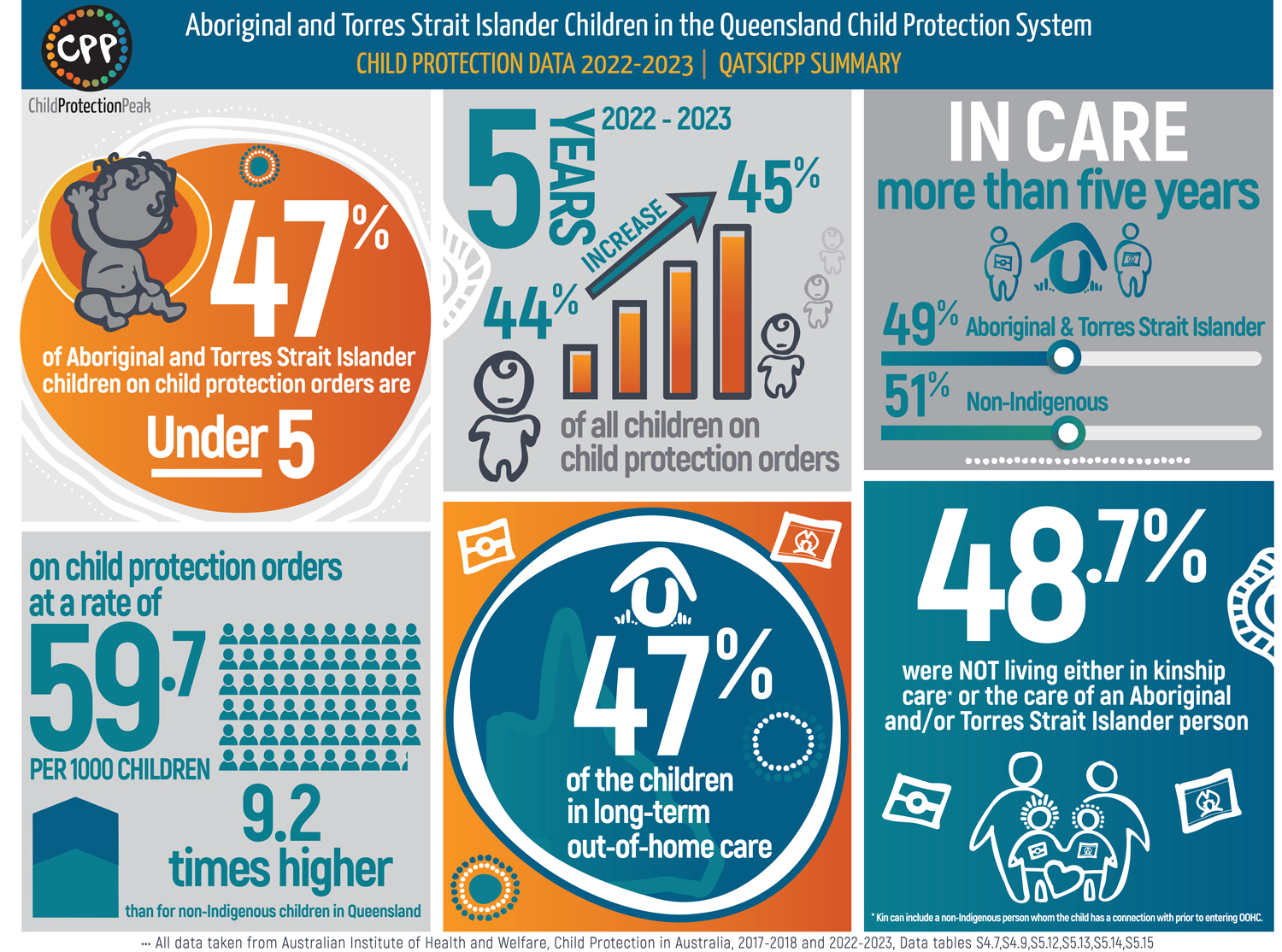
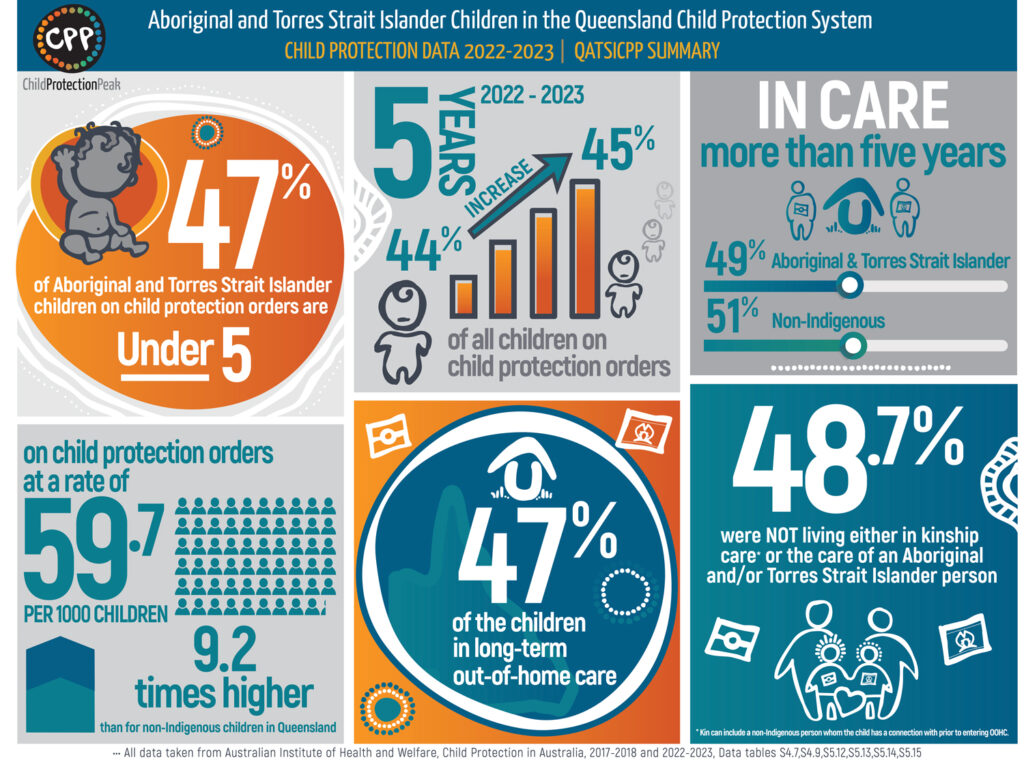
Queensland’s health crisis is not uniform. Brisbane’s median death age of eighty‑two contrasts with Far North regions at fifty‑two—highlighting stark inequality. First Nations children and those in remote communities face even worse outcomes, influenced by systemic barriers in access and prevention .
Such geographic and cultural demand tailored strategies. Dr Littlewood emphasised that universal models fail unless they adapt to local contexts.
Queensland Alarm : Urgent Reforms as Chronic Threatens Lifespan
Given that forty percent of Queensland’s health burden is preventable, there is growing consensus that current funding prioritises treatment over prevention. Experts are urging policymakers to pivot toward proactive care—offering lifestyle coaching, early intervention, and easy access to support systems.
Digital health pilots and targeted community programs have shown effectiveness. Scale‑up efforts may reduce emergency visits and chronic illness admissions, and in turn, improve life expectancy projections.
A Call to Action for Families and Policymakers
The message from forum speakers was clear: there is still time to avert this intergenerational health crisis. Prevention must start early, with families supported to make healthier lifestyle choices, and systems built for accessibility and affordability.
Parents voiced support, and community leaders called for policy backing. The phrase “We’ve got the best system here in the world, hands down, but the funding model does not help with prevention” summed it up.
Conclusion: Turning Alarm into Reform
Queensland’s startling new health data should not be a death sentence. Yet, without decisive reforms, the next generation faces shortened lifespans and chronic burdens. Systems that support prevention, equitable care, and workforce stability are critical.
The future will depend on whether Queenslanders heed the alarming signs as a wake‑up call—and act to protect the children who deserve healthier futures.